Hearing loss doesn’t wait for your retirement years. In fact, many adults begin to notice subtle—but significant—changes to their hearing as early as their 40s. Whether it’s missing punchlines at dinner parties or struggling to hear your kids in the backseat, these issues aren’t just frustrating—they can impact your work, relationships, and quality of life.
📈 Hearing Loss in Midlife: A Growing Concern
It’s a common misconception that hearing loss is only associated with aging into your 70s or 80s. However, studies show that roughly 1 in 5 adults in their 40s already have some measurable hearing loss, and the rate climbs to nearly 1 in 3 by age 59. Many adults chalk it up to background noise or “mumbling”—but the reality is often physiological.
Why It’s Happening Earlier:
- Increased exposure to recreational noise (earbuds, concerts, streaming)
- Longevity of workplace noise exposure from earlier life
- Rising rates of chronic conditions like diabetes and hypertension
- Better awareness and earlier diagnosis
👂 Types of Hearing Loss
Understanding the nature of hearing loss can guide diagnosis and treatment. Here’s a breakdown:
| Type | Underlying Cause | Reversible? | Common In |
|---|---|---|---|
| Sensorineural | Damage to hair cells in cochlea or auditory nerve | No; managed with hearing aids or implants | Most age-related cases |
| Conductive | Physical blockage or middle ear issue | Often yes; wax removal or surgery | Ear infections, wax issues |
| Mixed | Combination of the above | Partially | Older adults with chronic issues |
Sensorineural hearing loss is the most common type starting in midlife, and is typically permanent. That’s why catching it early is key.
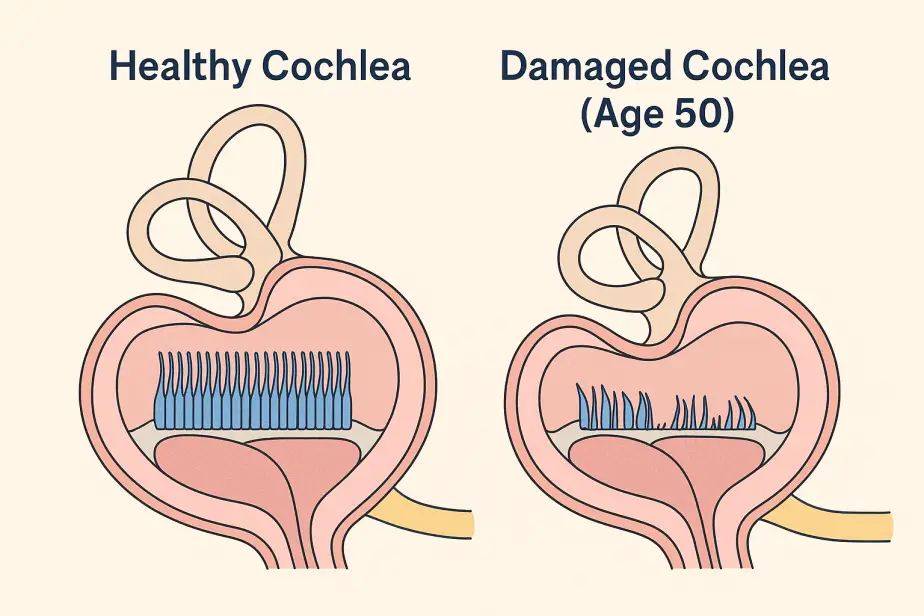
🧠 1. Age-Related Hearing Decline (Presbycusis)
Presbycusis is the medical term for the slow, bilateral (both ears) decline in hearing that comes with aging. This is not a sudden event—it’s a progressive, degenerative condition often starting in the high frequencies.
What’s Happening in the Ear:
- The outer hair cells in the cochlea, responsible for amplifying sound, begin to die off.
- The stria vascularis, which maintains ionic balance in the cochlear fluid, weakens, reducing cochlear performance.
- Neural pathways involved in auditory processing become less efficient.
Real-Life Impact:
- You hear that someone is talking but can’t distinguish the words.
- Background noise overwhelms speech clarity.
- Music sounds dull or distorted.
Patient perspective:
“I can hear my wife talking, but I can’t make out what she’s saying unless she’s facing me.”
Clinical Tip: Midlife patients often pass hearing screenings for low frequencies but fail at high frequencies—missing birdsong, beeping devices, or whispered speech.
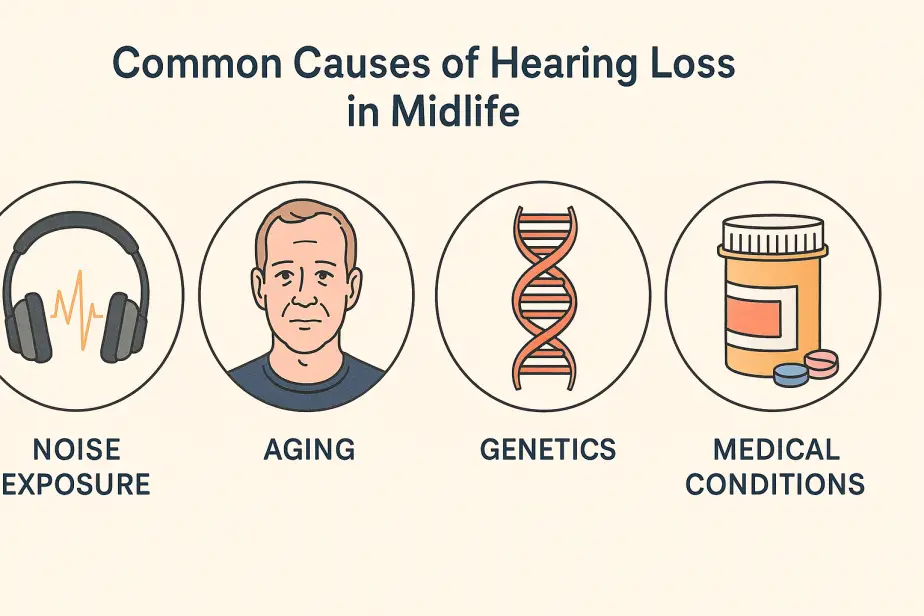
🎧 2. Noise-Induced Hearing Loss (NIHL)
Even if you never worked on a factory floor, chances are your ears have taken some abuse. Decades of personal audio devices, sports events, home improvement tools, and even loud gyms all contribute to hearing damage.
How NIHL Works:
- High-intensity sound damages cochlear hair cells.
- Repeated exposure accelerates cumulative damage.
- Tinnitus (ringing) is often the first symptom—even before hearing loss shows up on an audiogram.
Activities That May Have Contributed:
- Using headphones >85 dB (typical smartphone volume at 70%+)
- Attending concerts without ear protection
- Mowing lawns or snowblowing regularly without earmuffs
- Riding motorcycles or working in noisy environments
“If you walk away from an event with muffled hearing or ringing ears, your auditory system just took a hit.”
🧬 3. Genetic Predisposition
Hearing loss often runs in families—even when noise exposure and health factors are ruled out. Certain people inherit more fragile cochlear cells or accelerated metabolic aging of the auditory system.
What to Look For:
- Parents or siblings who needed hearing aids before age 60
- Similar patterns of early-onset tinnitus
- Family history of sudden hearing loss or autoimmune conditions
Genetics may not be destiny, but they certainly tilt the odds.
💊 4. Ototoxic Medications
Certain medications can harm your hearing, especially over long periods or in higher doses.
Ototoxicity Risk Drugs:
| Drug Class | Examples | Risk Level |
|---|---|---|
| Antibiotics | Gentamicin, vancomycin | High (esp. IV use) |
| Chemotherapy | Cisplatin, carboplatin | Very high |
| NSAIDs | Aspirin, ibuprofen (high dose) | Moderate |
| Diuretics | Furosemide, bumetanide | Moderate (esp. IV) |
| PDE5 Inhibitors | Viagra, Cialis | Low to moderate |
Signs of ototoxicity:
- Sudden or fluctuating hearing loss
- Tinnitus that appears during treatment
- Loss of balance or vertigo
Always report new hearing symptoms to your provider when starting a new medication.
🦻 5. Earwax, Otosclerosis & Other Conductive Causes
Sometimes the problem isn’t inner ear damage, but rather a mechanical issue.
Common Conductive Causes in Midlife:
- Impacted earwax: More common with hearing aid users or narrow ear canals.
- Otosclerosis: Abnormal bone growth around the stapes bone, leading to stiffness and reduced sound transmission.
- Eustachian tube dysfunction: Often triggered by allergies or sinus infections, creating pressure imbalances.
- Chronic ear infections: Can leave lasting scar tissue or fluid in the middle ear.
Pro Tip: Conductive losses are often treatable by ENT physicians, so don’t assume all hearing loss is permanent!
❤️ 6. Cardiovascular & Metabolic Health
Hearing health is closely linked to blood flow. The inner ear is supplied by the labyrinthine artery, which is extremely small and easily affected by systemic conditions.
Risk Factors:
- Hypertension: Reduces oxygenation to cochlear tissue.
- High cholesterol: May contribute to plaque buildup, reducing blood flow.
- Diabetes: Damages blood vessels and nerves, including those in the ear.
- Smoking: Constricts blood vessels, including those serving the auditory nerve.
If it’s bad for your heart, it’s probably bad for your ears too.
⚖️ 7. Hormonal & Autoimmune Causes
Women in Midlife:
- Estrogen decline during perimenopause can alter cochlear sensitivity.
- Some women experience tinnitus or a sensation of “fullness” in the ears during hormonal shifts.
Autoimmune Disorders:
- Conditions like lupus, rheumatoid arthritis, or autoimmune inner ear disease (AIED) can cause sudden or fluctuating sensorineural hearing loss.
- AIED typically presents with asymmetrical loss and may respond to corticosteroids.
Encourage a full medical evaluation if hearing loss is rapid or associated with systemic symptoms.
🧍♀️ 8. Lifestyle, Sleep & Stress
While often overlooked, lifestyle factors influence auditory health significantly.
Poor Sleep:
- Increases inflammation
- Reduces neural efficiency in auditory processing
Chronic Stress:
- Raises cortisol, which affects blood supply to the cochlea
- Can exacerbate tinnitus
Poor Nutrition:
- Low intake of magnesium, potassium, and B12 linked to auditory dysfunction
A healthy lifestyle supports not just your body but your ability to hear and communicate clearly.
🔎 Early Warning Signs
Many people in midlife normalize or dismiss their hearing struggles. Here’s what to watch for:
- Constantly asking people to repeat themselves
- Misunderstanding conversations, especially in groups
- Increased TV or phone volume
- Avoiding social settings due to difficulty hearing
- Tinnitus (ringing, buzzing, or hissing)
- Feeling fatigued after conversations
Action Step: Schedule a baseline hearing test with a licensed audiologist. It’s painless, affordable, and takes about 30 minutes.
👩⚕️ What You Can Do
- Schedule Regular Hearing Tests
Start in your 40s. Repeat every 2–3 years unless you notice a change. - Limit Noise Exposure
Use musician-grade earplugs in loud environments. Invest in noise-canceling headphones. - Control Health Conditions
Manage blood pressure, diabetes, and cholesterol aggressively. - Explore Hearing Technology Early
Modern hearing aids are nearly invisible, Bluetooth-enabled, and can enhance your life long before severe loss sets in. - Stay Socially Engaged
Untreated hearing loss is linked to depression and cognitive decline. Staying connected keeps your mind sharp.
🧠 Hearing Health = Quality of Life
Your 40s and 50s are a time to invest in your future health—including your hearing. The earlier you identify and manage hearing changes, the better your outcomes for communication, cognition, and emotional well-being.
Don’t wait for it to become a major problem. Take the first step today (see a clinic near you).