Quick take: A videonystagmography (VNG) is the most commonly ordered vestibular test battery. Wearing light-sealed video goggles, your eye movements are recorded while you follow targets, change head/body positions, and—during caloric testing—while warm and cool air (or water) gently changes the temperature in each ear canal. These controlled conditions help your care team determine whether one or both inner ears (the vestibular system) are contributing to dizziness, vertigo, imbalance, or visual blurring.
VNG has largely replaced ENG (electronystagmography). Both evaluate the same physiologic responses, but VNG uses infrared cameras while ENG uses skin electrodes. Cameras are more comfortable, more precise, and easier for clinicians to calibrate—so few clinics still use ENG.
What VNG (and Rotary Chair) Are Looking For
VNG evaluates how the vestibular system (semicircular canals and their neural pathways) senses rotation and acceleration and how that information is integrated with vision and proprioception. Your brain expects symmetrical input from the right and left ears. If one side is weaker or inhibited—or if central pathways are affected—the brain receives conflicting signals, often perceived as vertigo (spinning), lightheadedness, oscillopsia (bouncing vision), or unsteadiness.
Rotational chair testing, when included, complements caloric testing by assessing the vestibulo-ocular reflex (VOR) across a broader range of frequencies (from very slow to faster head movements encountered in daily life).
What to Expect at the Appointment
How Long Does VNG Take?
Plan on ~90 minutes for a standard VNG. If a full vestibular battery is ordered (e.g., VEMP, posturography, rotational chair), it can take up to 3 hours. A typical flow looks like this:
- 20 minutes – Detailed vestibular case history
- 20–30 minutes – Hearing evaluation (sometimes done at a prior visit)
- 10 minutes – Goggles placement & calibration
- ~20 minutes – Oculomotor tests
- ~15 minutes – Positional/positioning tests (including Dix–Hallpike for BPPV)
- ~30 minutes – Caloric testing (warm & cool stimuli in both ears)
Optional/adjunct tests (if ordered):
- ~20 minutes – Computerized Dynamic Posturography (CDP)
- ~20 minutes – VEMP (Vestibular-Evoked Myogenic Potentials)
- ~3 minutes – High-Frequency Headshake test
- ~30 minutes – Rotational Chair (SHA and step/trapezoid protocols)
- ~10 minutes – Static Subjective Visual Vertical (SVV)
Below is a deeper dive into each element so you know exactly what happens and why it matters.
The Vestibular Case History (Why It’s Critical)
Your audiologist will start with a thorough history. Detailed answers help pinpoint whether symptoms are more consistent with peripheral (inner ear), central (brain/brainstem/cerebellum), or multifactorial causes, and guide which tests/interventions will be most useful.
Common Symptom Questions
- Do you experience spinning, tilting, or a sense of falling to one side?
- Do episodes occur in attacks? How often and how long do they last? When was the first episode?
- Are you symptom-free between attacks?
- Do hearing changes (fullness, ringing, hearing loss) accompany attacks?
- Are symptoms triggered by standing up, position changes, or lying down?
- Any recent cold/flu? Head trauma?
- Do you have nausea, vomiting, or motion sensitivity?
- Any neurologic symptoms (double vision, limb weakness, slurred speech, numbness, severe headache)?
Lifestyle & Medical Factors Often Reviewed
- Recent eyeglass prescription changes, stress, sleep, hydration, caffeine/alcohol use
- History of migraine, diabetes, thyroid disease, blood pressure issues
- Medications that can affect the inner ear or central processing (see prep section below)
- Family history of migraine, vestibular disorders, or metabolic conditions
What Each VNG/ENG Component Measures
1) Oculomotor Tests
You’ll follow a moving dot (smooth pursuit), jump your eyes between targets (saccades), and sometimes view moving patterns (optokinetics). The goggles track precise eye movements.
What it tells us: Abnormal pursuit/saccades typically suggest central pathway involvement (brain/brainstem/cerebellum). Normal oculomotor function helps isolate later findings to the peripheral system.
2) Positional & Positioning Tests
In a darkened environment, you’ll be placed in standard positions (back, sides, head turns). The system records any nystagmus (involuntary eye movements) at rest.
Dix–Hallpike maneuver is then used to evaluate BPPV (Benign Paroxysmal Positional Vertigo). If otoconia (“ear crystals”) have migrated into a semicircular canal, changing your head position may briefly provoke vertigo and a characteristic nystagmus pattern.
What it tells us: Identifies static asymmetries and positional triggers; flags BPPV, which is very treatable with canalith repositioning maneuvers (e.g., Epley).
3) Caloric Testing
While you recline ~30°, warm and cool air (or water) are delivered to each ear for ~60 seconds. Temperature changes create a mild convection current in the horizontal canal, temporarily simulating head rotation. Many people feel transient spinning; it typically resolves within minutes.
- Fixation suppression: A brief light is presented to see whether visual fixation reduces the nystagmus response (a central function).
- Tasking: You’ll be asked simple questions during recordings to keep brain activity consistent for accurate responses.
What it tells us: Compares right vs. left canal function at a very low frequency of stimulation. Key metrics include unilateral weakness and directional preponderance. Marked asymmetry suggests a peripheral vestibular hypofunction on the weaker side.
4) Rotational Chair (If Ordered)
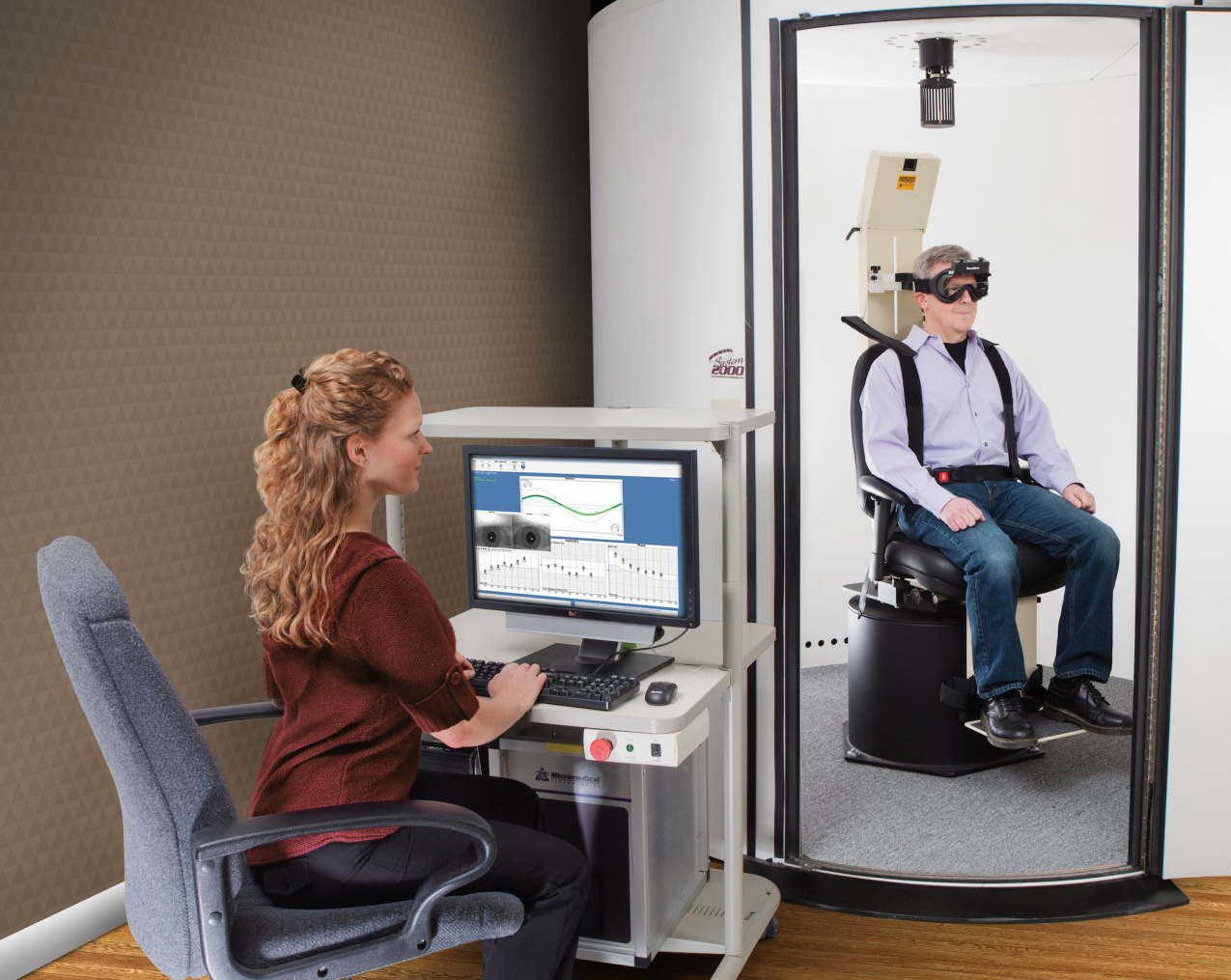
SHA (Sinusoidal Harmonic Acceleration): The chair gently oscillates at increasing speeds/frequencies. This assesses the VOR from ~0.01 to 2 Hz.
Step (Trapezoid) Test: The chair accelerates to a constant velocity (e.g., 60°/s or 240°/s) and then stops abruptly. The decay of eye velocity provides time constants and asymmetry measures; large asymmetry often mirrors caloric findings.
Visual Enhancement/Suppression: Compares responses when you fixate a target or enhance visual-vestibular interaction.
What it tells us: Complements calorics by measuring VOR performance at physiologic head-movement speeds. Helpful when calorics are inconclusive, when both ears are reduced (bilateral hypofunction), or when confirming central involvement.
VEMP (Vestibular-Evoked Myogenic Potentials)
Assesses otolith (typically saccule/inferior nerve) function using a loud tone burst (~95 dB) while you activate the sternocleidomastoid muscle (turn and slightly lift your head). Note: Absent VEMPs can be age-normal in older adults.
Computerized Dynamic Posturography (CDP)
With a safety harness, you stand on a platform while visual/under-foot conditions change across six subtests. Some trials use a sway-referenced platform or visual surround. This quantifies how you weight somatosensory, visual, and vestibular inputs to maintain balance.
Static Subjective Visual Vertical (SVV)
A line is presented in darkness. You adjust it to what appears perfectly vertical. Normal is within approximately ±2.5° of true vertical; larger errors suggest utricular pathway involvement.
How Results Are Interpreted
- Oculomotor: Abnormal pursuit/saccades/OKN → consider central involvement.
- Positional: Presence/absence and direction of nystagmus help localize peripheral vs. central and identify BPPV canal involvement.
- Calorics: Unilateral weakness quantifies side-to-side differences; directional preponderance reflects bias. Abnormal fixation suppression suggests central issues.
- Rotational chair: VOR gain, phase, and symmetry across frequencies; time constants on step tests (e.g., markedly short <10 s or long >30 s).
- VEMP/SVV/CDP: Add otolith and functional balance context to complete the picture.
When you’ll get results: Many clinics need time (often a few days) to analyze and correlate all data points. If findings are clearly normal or point to a straightforward diagnosis (e.g., classic BPPV), your clinician may discuss results the same day.
How to Prepare (Read This Before Your Test)
It’s essential to follow prep instructions so your results are accurate. Unless your physician tells you otherwise, typical guidance includes:
- Avoid vestibular-suppressant meds for at least 48 hours (see lists below). Do not stop blood pressure, seizure, diabetes, or other essential medications without prescriber approval.
- No heavy meals for 4 hours before testing. If needed for medical reasons, eat lightly.
- Come with a clean, makeup-free face so goggles can seal and track pupils accurately.
- Dress comfortably.
- Arrange a ride, if possible. You may feel fatigued or mildly off-balance afterward.
Medications Commonly Held 48 Hours Before Testing*
*Only with prescriber approval when applicable.
Anti-anxiety / Sedative-Hypnotic (examples)
- Diazepam (Valium), Lorazepam (Ativan), Alprazolam (Xanax)
- Prochlorperazine (Compazine)
Anti-vertigo / Motion Sickness
- Meclizine (Antivert, Bonine), Dimenhydrinate (Dramamine)
- Promethazine (Phenergan)
- Scopolamine patch
- Diazepam (Valium), Prochlorperazine (Compazine)
Antihistamines (examples)
- Diphenhydramine (Benadryl), Chlorpheniramine (Chlor-Trimeton)
- Many OTC cold/allergy combinations (check labels)
Do not discontinue medications for blood pressure, seizures, diabetes, thyroid, or other chronic conditions without guidance from your prescriber.
Safety, Comfort, and Contraindications
- VNG is non-invasive. Calorics and rotational testing may temporarily provoke dizziness or nausea; this is expected and short-lived.
- Let your clinician know about recent eye surgery, severe neck/back limitations (which may affect positioning tests), perforated eardrum or recent ear surgery (important if water calorics are planned), or panic disorder (we can add extra breaks and reassurance).
- Tell us if you are pregnant or have migraine; accommodations can be made.
After the Test
It’s common to feel a bit tired or “off” for an hour or two. Most people can resume normal activities the same day. Your audiologist will outline next steps, which could include canalith repositioning for BPPV, vestibular physical therapy, additional imaging or neurology/otology referral, or a home exercise program focused on VOR and balance retraining.
Frequently Asked Questions
Is VNG the same as ENG?
They test the same physiology, but VNG uses cameras and ENG uses skin electrodes. VNG is now standard due to comfort and accuracy.
Will VNG make me sick?
You may feel brief spinning during calorics or queasiness with rotational testing. Symptoms usually fade within minutes. Let your clinician know if you need extra breaks.
Can I drive afterward?
Many patients can, but if you still feel off-balance, arrange a ride to be safe.
What conditions can VNG help diagnose?
BPPV, vestibular neuritis/labyrinthitis, Meniere’s disease, bilateral hypofunction, vestibular migraine, and clues to central disorders when oculomotor or fixation suppression are abnormal.
What if my results are “normal” but I’m still dizzy?
Normal VNG doesn’t rule out all causes (e.g., vestibular migraine, PPPD, orthostatic intolerance). Your care team may recommend additional testing or therapy.
Helpful Resources
- Vestibular Disorders Association (VeDA) – patient-friendly education and support
- NIDCD (NIH) – research-backed information on balance and hearing
Pre-Test Checklist (Print or Screenshot)
- Held vestibular-suppressant meds for 48 hours (if approved by prescriber)
- No heavy meal within 4 hours (light snack if medically necessary)
- Face clean; no eye makeup/lotions around eyes
- Comfortable clothing; bring glasses if you wear them
- Transportation arranged (recommended)
- List of medications and symptom timeline
About the Author
Jonathan Javid, AuD, is a clinical audiologist with 12+ years of experience, including extensive work in vestibular and hearing care. He is the founder of HearingInsider.com, where he writes patient-first, evidence-informed guides on hearing and balance.